Study warns that SARS in pregnant women increases by four times the risk of fetal death
24/05/2023
Clarissa Viana (Cidacs/Fiocruz Bahia)
What are the impacts of the most serious cases of COVID-19 on pregnancy? According to an article published in the journal BMC Pregnancy and Childbirth, the chance of fetal death was four times higher in pregnancies during which women had Severe Acute Respiratory Syndrome (SARS). This risk increased even further when the clinical condition of SARS in the pregnant woman was accompanied by vaginal delivery (risk 7.06 times greater), or when it was necessary to hospitalize the pregnant woman in the Intensive Care Unit – ICU (risk 8.79 times greater) or use mechanical ventilation (risk 21.22 times greater).
According to the research, the greater the severity of the clinical condition, the greater the chance of losing the baby (image: Cidacs/Fiocruz Bahia)
To investigate the association between the risk of fatal death and SARS during pregnancy, researchers monitored pregnant women who required hospitalization with respiratory symptoms in the state of Bahia. The study was carried out based on the integration of data from the Live Birth Information System (Sinasc), the Mortality Information System (SIM) and the Severe Acute Respiratory Syndrome Epidemiological Surveillance System (Sivep).
According to the investigation, the greater the severity of the clinical condition, the greater the chance of losing the baby. “The risk increased according to the severity of the clinical condition, for example, if the pregnant woman needed to be admitted to the ICU, or to breathe with the help of devices, the chance of fetal death was 8 to 21 times greater”, explains the researcher who led the study, Rita Carvalho Sauer, employee of the Epidemiological Surveillance at the East Regional Health Center, of the State Department of Health of Bahia, and doctoral student in Epidemiology at the Collective Health Institute of the Federal University of Bahia.
Due to the greater metabolic demand of carrying a fetus, in general, pregnant women are less tolerant to a lack of oxygen in the blood. “If the lung function of the pregnant woman is impaired by the severe acute respiratory syndrome, the oxygenation of the fetus may be deficient, leading to fetal distress and even death”, she explains.
The findings indicate the need for careful monitoring of cases of infection to avoid possible complications, as well as the adoption of preventive measures during childbirth. “Vaginal delivery in women with severe acute respiratory syndrome also increased the chance of fetal death, probably because childbirth demands a large amount of energy from the mother's body”, states the researcher. Cesarean delivery in pregnant women with SARS was not associated with fetal death, however, further studies are needed to assess the survival rate of these newborns.
Importance of prevention
The researchers warn of the need to prioritize pregnant women in preventive actions against the SARS-CoV-2 and other respiratory viruses. Actions such as avoiding contact with ill people, staying up-to-date with the vaccines and wearing masks whenever being in crowded environments is necessary are simple precautions that can prevent major problems for pregnant women and their babies.
“COVID-19 can be dangerous at any time during pregnancy, but this study showed that most cases of severe acute respiratory syndrome occurred in the third trimester of pregnancy. This finding alerts the need for greater care, especially from the 27th week of pregnancy onwards”, highlights Rita.
Pregnant women are more prone to complications from viral infections, such as secondary bacterial infections, disseminated intravascular coagulation and multiple organ failure. Moreover, COVID-19 during pregnancy may favor the occurrence of clotting problems in the mother and increase the risk of placental injuries.
“If the pregnant woman has respiratory symptoms, even if they are mild, it is very important that she seek medical care and that she is properly assessed, treated and monitored until she gets better. And, in the face of any symptom of respiratory discomfort or shortness of breath, the pregnant woman needs to seek emergency care as soon as possible, so that the medical team can assess which interventions will be necessary to avoid more serious complications”, she emphasizes.
Methodology
During the period analyzed (January 2019 to June 2021), 479,038 births, 333 deaths of pregnant women, and 6,841 fetal deaths, in addition to 13,077 women of reproductive age who had SARS were reported. Cases of Severe Acute Respiratory Syndrome that occurred in the period prior to the COVID-19 pandemic and fetal deaths that occurred simultaneously with the death of the pregnant woman were excluded.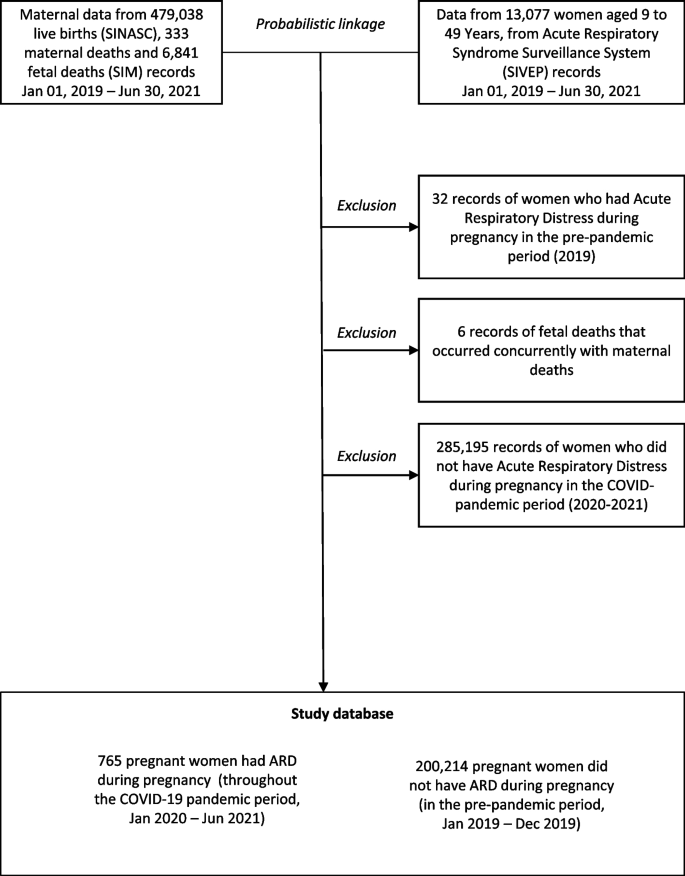
After the data integration process, 765 women who had SARS during pregnancy during the COVID-19 pandemic were identified, considered as an “exposed group”. These women had severe respiratory symptoms such as fever and cough, accompanied by dyspnea, low oxygenation and respiratory failure. The “non-exposed group” was formed by women who were pregnant in the period prior to the pandemic (in 2019) and did not have severe respiratory problems (SARS) – a total of 200,214 pregnant women.
The two participating groups – with and without SARS – were formed mainly by women aged between 20 and 35 years (65.9% and 70.1%), mixed race (75.5% and 76.6%), with secondary education incomplete (59.3% and 62%) and single (64.4% and 52.7%), respectively. Among the 765 pregnant women who were hospitalized with Severe Acute Respiratory Syndrome, 37.38% (286) were referred to the Intensive Care Unit and 16.6% (127) required mechanical ventilation.
Sociodemographic variables such as education level, race/color, marital status and human development index (HDI) of the municipality of residence were included. Additionally, the characteristics of the pregnancy were analyzed, such as the type of pregnancy (a single fetus, twins or more); number of previous pregnancies; sex of the fetus; type of delivery (vaginal or cesarean section), presence of fetal congenital anomalies, gestational age in weeks, and whether there was fetal death.
The study had the participation of researchers from the State Department of Health of Bahia, the Institute of Collective Health of UFBA, the Center for Data and Knowledge Integration for Health (Cidacs/Fiocruz Bahia), the University of Recôncavo da Bahia (UFRB) and the London School of Hygiene and Tropical Medicine.