Study suggests persistent infection by zika virus in the placenta
18/12/2020
Maíra Menezes (IOC/Fiocruz)
Most times a pregnant woman goes through a viral infection, such as a common cold, the baby remains protected in the womb. This protection is provided by the placenta, the organ that connects mother and baby and works as a barrier against microorganisms. However, there are pathogens that can overcome this barrier. One example is the zika virus. In 2015 and 2016, it caused a public health emergency of international relevance due to its association with microcephaly.
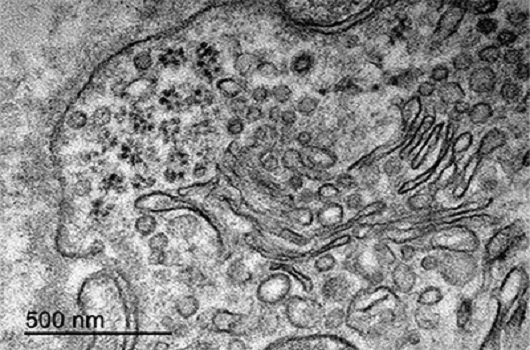
Months after infection, a cluster of particles of a size compatible with the Zika virus was observed within the placenta cells of an infected pregnant woman (Photo: Rabelo et al.)
In the search for answers about the disease, research led by the Oswaldo Cruz Institute (IOC/Fiocruz) and by the University of the State of Rio de Janeiro (UERJ) is now focusing on this key organ. Published in Frontiers in Immunology, the study analyzed samples of the placentas of ten patients who got the disease during pregnancy. The researchers observed that the virus causes a persistent infection in the organ, leading to inflammation, vascular dysfunction, and severe tissue damage. In cases of microcephaly, the study also found a significant reduction of a substance produced in the placenta, called brain-derived neurotrophic factor (BDNF), essential for the development of the fetal nervous system.
“We confirmed the presence and replication of the zika virus in various placental cells and proved a robust inflammatory environment that may remain for months, as the virus continues to replicate in the organ. The infection leads to pathological changes in the tissue, and in some cases, they can make it hard to maintain the pregnancy and hamper fetal development”, states Marciano Viana Paes, researcher of the Interdisciplinary Laboratory of Medical Research of the IOC and coordinator of the study. “The persistent infection also increases the chances of having the virus get to the fetus, and may regulate neurotrophic factors produced in the placenta, related to damages in the development of the fetal brain”, completes the first author of the study, Kíssila Rabelo, who developed the research during a doctorate in Clinical and Experimental Physiopathology at UERJ, under the guidance of UERJ professor Jorge José de Carvalho and co-tutored by Paes.
Various research groups and maternal-infant assistance units in Rio de Janeiro collaborated with this work. The study was coordinated by the Interdisciplinary Laboratory of Medical Research of the IOC and by the Laboratory of Ultrastructure and Tissue Biology of UERJ. Other participants were: IOC Viral Immunology Laboratory, National Institute of Women, Children and Adolescents Health Fernandes Figueira (IFF/Fiocruz), Center for Technological Development in Health (CDTS/Fiocruz), Federal University of the State of Rio de Janeiro (Uni-Rio), Federal University of Rio de Janeiro (UFRJ), Medical School of Campos, and Reference Center for Immuno-Infectious Diseases (CRDI), in addition to units of the IMNE group in the city of Campos dos Goytacazes, the Dr. Beda General Hospital, Ceplin, and Nicola Albano Neonatal ICU. The project relied on funding by the National Council for Scientific and Technological Development (CNPq) and by the Carlos Chagas Foundation for Research in Rio de Janeiro (Faperj).
Infection and Inflammation
The research analyzed different samples from ten cases of zika in pregnant women, reported in 2015 and 2016, at the peak of the outbreak of zika. Five patients gave birth to microcephalic babies and five had children with normal head size. The placenta samples were collected after labor and were compared to those of five pregnant women who had not been infected (control group).
The study shows ample evidence that the zika virus remains in the placenta and replicates in the organ, months after contagion. Signs of the presence of the virus were found in all the samples, including the cases in which the patients had shown symptoms of the disease, such as fever and skin rash, during the first trimester. In addition, clusters of viral particles were detected inside placental cells. Damages in cell organelles were also observed for the very first time.
The study provides details on the inflammatory process triggered by the zika virus in the placenta. The work also shows an increase in inflammatory substances that activate the immune response and in defense cells that fight the infection. However, the immune reaction cannot eliminate the zika, and the excessive inflammation generates a toxic environment for placental cells.
“We observed that some patients show a persistent infection in the placenta, and even then they do not develop antibodies that neutralize the zika virus. The immune response against the infection includes various cells of the immune system, such as macrophages and T CD8+ lymphocytes, and has a more cytotoxic profile, with the involvement of cytokines [molecules that provide signaling between cells] that lead to tissue damage and increased vascular permeability”, says Rabelo.
Zika proteins and genetic material were found in six different cell types, as well as in placental defense cells. The findings strengthen the conclusions of previous studies, pointing to two possible infection pathways in babies. On the one hand, the progressive transmission of the virus between placental cells until it reaches the amniotic fluid and then the fetus. On the other hand, the transportation of viral particles by immune cells, which are passed from mother to baby.
Neurotrophic factor
By comparing the samples, researchers found that the BDNF substance showed a statistically significant reduction in the cases of microcephaly. Produced in the placenta, this molecule promotes neuron growth and differentiation during fetal development and is fundamental for the formation of the brain. According to the scientists, although it does not work alone, it may be one of the determining proteins for the severity of the lesions, and BDNF levels in the placenta may serve as a predictive marker of damage extension.
“BDNF is a neurotrophic factor normally produced in the placenta to maintain placental cells, but it is also essential for the development of the fetal nervous system. This is why we investigated its presence in the different samples. We observed a reduced expression of BDNF in the infected tissues and almost no expression in the placentas that generated babies with microcephaly. This shows that in addition to the direct infection of the fetus, the zika virus can also affect proteins produced in the placenta, leading to damages on the development of the fetal nervous system”, explains Paes.
Response to society
Between 2015 and 2016, the zika virus caused almost three thousand cases of the congenital syndrome, including microcephaly and other malformations, in addition to fetal and newborn deaths. The public health emergency had its end declared as the number of cases progressively declined, but the disease has not gone away. According to the Ministry of Health, new cases continue to occur systematically in the country. Specialists also say that new outbreaks can occur in the future.
“In 2015 we saw the rapid dissemination of the zika virus in Brazil and the situation of pregnant women who were informed on congenital syndrome and had to take care of babies with severe disabilities. This was very shocking and made us think about how the scientific community could know so little about this disease. As a research group that already works with arboviruses, we dedicated our efforts to understanding the pathogenesis of this disease, which was little known until then”, states Rabelo.
“Establishing the profile of the infection and of the immune response caused by the zika virus in the placenta is an important foundation to detect plasmatic markers and for the development of drugs and vaccines, as well as for other studies that hope to clarify how the disease occurs. We, therefore, hope to contribute, together with the entire scientific community, to minimize the harm to the population that still suffers from the disease”, concludes Paes.