Covid-19: new evidence on the impact of the virus on blood
27/07/2020
Maíra Menezes (IOC/Fiocruz)
A study led by the Oswaldo Cruz Institute (IOC/Fiocruz) and by the Federal University of Juiz de Fora (UFJF), in collaboration with hospitals and research centers in Rio de Janeiro, provides new information that helps understand one of the most severe and frequent complications observed in Covid-19 patients hospitalized in intensive care units (ICUs). Published in “Blood”, the main international scientific journal in the area of hematology and coagulation, the study focuses on the impact of the virus in the blood, and draws particular attention to platelets, fundamental for the coagulation process.
Although the coronavirus affects mainly the lungs, previous evidence had already showed that in severe cases, Covid-19 also alters blood coagulation processes. These patients often present excessive coagulation, with the formation of blood cell and protein aggregates that are called thrombuses (or blood clots). Blood clots can interrupt circulation, leading to thrombosis, heart attacks, or pulmonary embolism, associated to more serious cases and to fatal cases as well.
“Health professionals are closely following the evolution of severe cases, with an eye out for thrombotic events. Our study focused on understanding how, in these patients, the virus interferes on the early stages of the cascade of processes that trigger coagulation. Platelets play an important role in these processes”, summarizes Eugênio Hottz, professor at the Federal University of Juiz de Fora (UFJF), collaborating researcher of the IOC’s Immunopharmacology Laboratory, and leading author of the paper.
To investigate the mechanisms involved in this process, researchers analyzed and compared samples of blood and of the respiratory tract of patients with different presentations of Covid-19, including severe patients that had to be maintained in intensive care units (ICUs), patients with mild manifestations, and asymptomatic ones. Samples of healthy individuals were also included in the study, for comparison purposes.
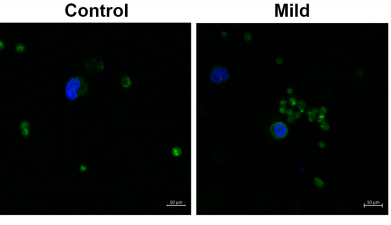
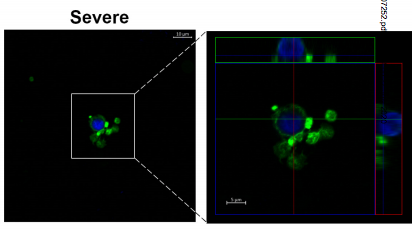
The analysis made using flow cytometry and microscopy techniques intended to identify, in the different samples, which alterations could be observed in the platelets and the factor activation cascade that lead to coagulation, something that takes place at a molecular level. Samples were collected from patients early in their hospital stay, and the patients were followed throughout their hospitalization, so that the evolution of the case in the hospital could be associated to laboratory findings from the point of view of virus impact on blood dynamics.
According to the experiments, in patients with severe forms of Covid-19 there was an increase in platelet activation, and researchers also observed intense aggregation of platelets and monocytes, cells that act in the defense against infections - which did not happen in the samples obtained from patients with mild symptoms or no symptoms at all. The researchers were able to map two molecules that have a marked action in this adhesion process between platelets and monocytes: CD62P and αIIb/β3. In addition the study also showed that platelet activation induces monocytes to express a protein, called tissue factor, which triggers the entire coagulation process.
Comparing the results obtained in the lab and the outcome of patients followed throughout the study, both the levels of platelet activation and those of tissue factor expression in monocytes were associated to the severeness of the clinical status and to the prognosis of the disease, with a higher probability of evolution to mechanical ventilation and also to death among those with higher activation. “Our results show that platelet activation and their association to monocytes, with the formation of platelet-monocyte aggregates, are important for the triggering of blood coagulation”, states researcher Patrizia Bozza, chief of the IOC’s Immunopharmacology Laboratory and coordinator of the study.
Two fundamental points stem from the new evidence found by the team led by Hottz and Patrícia Bozza. The first one is the possibility that following platelet activation levels among hospitalized patients may serve as a kind of “sign” that a certain individual is more likely to evolve towards an unfavorable outcome, which may be an important element in decision-making for the medical staff, regarding certain approaches to be adopted. The second point is that, as we get to know the molecules involved in the adhesion between platelets and monocytes during the infection by the new coronavirus, drugs already available to inhibit platelets can be tested as therapeutic alternatives.
“Our results show that platelet activation takes place in severe cases of Covid-19. We still don’t know whether platelet activation worsens the situation or if this activation is just one of the many processes involved in the infection by the virus. In any case, monitoring platelet activation as a mark to indicate potential worsening is already a laboratory-based conclusion that can be adopted in clinical management of patients”, Hottz summarizes.
The paper suggests that the great release of inflammatory mediators in the plasma of patients with serious cases of Covid-19 may be one of the causes of the more intense activation of platelets in these people. It also points to the fact that inhibiting molecules that act in the process of adhesion and signaling between platelets and monocytes may interrupt the expression of tissue factor, paving the way to possible new therapies. In this sense, monoclonal antibody Abciximab, already widely used to avoid the formation of clots after surgeries, was one of the substances successfully tested by in vitro studies. “These results open the possibility of continuing with the investigation to identify therapies that can act on platelet activation events in Covid-19 cases”, says Patrícia Bozza.
“Since the beginning of the pandemic there have been reports of coagulation alterations, especially with thrombotic events in severe patients. This is a major concern for all healthcare teams treating severe Covid-19 patients. Identifying the factors that cause these alterations is crucial to establish new therapies for these patients. The collaboration between basic research and clinical research groups was fundamental to answer to these questions”, summarizes researcher Fernando Bozza, who works ad the Evandro Chagas National Infectiology Institute (INI/Fiocruz) and at the Instituto D’Or.
Translational and collaborative research
With experience in studies on thromboinflammatory response, the IOC’s Immunopharmacology Laboratory has focused mainly on diseases caused by arboviruses, and has had significant findings on the role played by platelets in severe cases of dengue fever in the past few years. When the Covid-19 emergency began, the team joined their efforts with those of scientists from different institutions in order to come up with a translational study, integrating clinical and laboratory data in the search for answers.
“The translational character of the research is result of a multidisciplinary team involving different research institutions and hospitals. This has allowed us to make an early assessment of samples obtained from patients, to identify cellular profiles, and to correlate laboratory findings and clinical aspects. This translational, multidisciplinary, multicentric approach allows us to associate laboratory information to what is taking place from a clinical standpoint”, highlights Eugênio Hottz.
In addition to IOC and UFJF, other participants in the study were the Center for Technological Development in Health (CDTS/Fiocruz), the Evandro Chagas National Institute for Infectious Diseases (INI/Fiocruz), the Paulo Niemeyer State Institute for the Brain, and D’Or Institute of Research and Teaching. The research was funded by the Carlos Chagas Filho Foundation for Research in the State of Rio de Janeiro (FAPERJ), the Inova Fiocruz Progarm, the National Council for Scientific and Technological Development (CNPq), the Coordination for the Improvement of Higher Education Personnel (Capes), and the D’Or Institute.